Frequently Asked Questions about Vasectomy
Traditionally, a local anesthetic has been injected into the skin and alongside each vas tube with a very fine needle, as small as diabetics use to inject themselves with insulin. One could feel a tiny poke in the skin, then a bit of a squeeze as the anesthetic was applied to each vas tube. However, most people do not like needles of any size ... especially there!

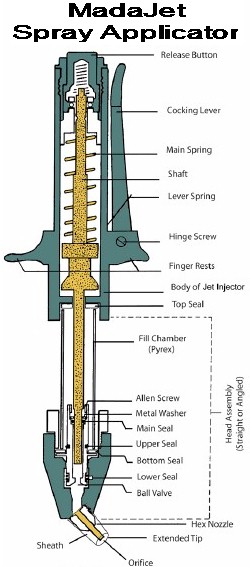
The spray penetrates to
about 3/16", enveloping
the vas.
A MadaJet® is a spray applicator which delivers a fine stream of liquid anesthetic at a pressure great enough to penetrate the skin to a depth of about 3/16", deep enough to envelop the vas tube held snugly beneath the skin. Each vas is positioned in turn beneath the very middle of the front scrotal wall and given two or three squirts. That numbs the skin and both vas tubes adequately for 99% of men. The other 1% (usually men who have thick skin or scarring due to prior surgical procedures in the area) will require a bit more anesthetic delivered with a fine needle, usually with no pain at all because of the partial anesthesia achieved with the MadaJet.
The spray penetrates to about 3/16", enveloping the vas. For "techies," the MadaJet is a rather simple but precisely machined device. A cocking lever lifts a piston (shaft) to a locked position, compressing a strong main spring and drawing anesthetic from a fill chamber into a cylinder at the bottom of a head assembly. When a release button is pressed, the spring forces the piston down into the cylinder, ejecting the anesthetic under high pressure through a tiny orifice at the end of an extended tip. A MadaJet is demonstrated (nothing graphic) in Dr. Stein's counseling video.Hemoclip
Some men request that we use a suture rather than a hemoclip out of an intuitive preference to avoid having any metal implanted in their bodies. No problem. A suture can take a minute more to apply than a hemoclip and may cause a little more local inflamation and scarring, but this is of little clinical significance, just an observation made at the time of vasectomy reversal, where we see virtually no scarring associated with clips because metal is so inert.
Below are artists' renditions of use of a clip and use of a suture to accomplish fascial interposition (separation of the ends). Removal of a small section of the testicular end is optional; we do not usually remove a piece because doing so reduces the degree of end separation.


45% of men took no pain medication following their vasectomies, not even the Tylenol that was provided. They had so little discomfort that they saw no need to take anything.
15% of men took pain medication (the Tylenol that was provided or home supplies of ibuprofen) one time "just in case", that is, as a precaution to prevent expected discomfort, not because they needed it.
29% of men took pain medication one time for discomfort, then did not need any additional doses.
11% of men took pain medication more than one time (two or three times), though at least 4 of these 11 men said that they had taken it more to prevent expected pain than because they were actually having discomfort.
0% of these men felt that they needed something stronger than Tylenol or ibuprofen, but we are asked for a prescription medication by about 1 in 500 men.
Dr. Stein has performed open-ended vasectomies exclusively since late 1990, and while there is some merit to this technique, the web pages lauding it are probably overstating the benefits.
First, not all open-ended vasectomies result in a sperm granuloma at the vasectomy site. Dr. Stein has reversed vasectomies for a number of his own vasectomy patients and learned that many of the lower ends simply end as a sealed tube with little or no surrounding inflammation. So a natural seal of the lower vas end must occur soon after an open-end vasectomy in many patients.
Second, some open-end vasectomy patients (about one in 50) will still develop post-vasectomy discomfort and tenderness of the epididymis. The likelihood of this occurring is lower with the open-end technique: 2% of patients as opposed to 6% of patients with the closed-end technique (Contraception 46(6):521-521, 1992). This "congestive epididymitis" usually responds quickly to an anti-inflammatory drug like ibuprofen, but serves as proof that an open-end technique is not a sure way to avoid post-vasectomy epididymal inflammation.
Third, a vasectomy site granuloma can be just as tender as epididymal inflammation, though it too usually responds quickly to anti-inflammatory drugs.
Fourth, while reversal success rates may be better after open-end vasectomies, performance of this technique is no guarantee of reversal success and many men with closed-end vasectomies have undergone successful reversals.
In summary, while an open-end technique offers theoretical benefits, use of it is not a "standard of care" and the closed-end technique has worked well for years.
The February 17, 1993 issue of the Journal Of The American Medical Association contained 2 studies (by the same research group) that suggest that vasectomy was associated with a small increased risk of prostate cancer in their study groups (almost 30,000 patients in 1 study and almost 40,000 patients in the other study). Because the question was initially raised by 2 studies back in 1990, the World Health Organization convened a 1991 meeting of 23 international experts to review all research regarding vasectomy and prostate cancer. They concluded that there was no plausible biologic mechanism for a relationship between vasectomy and prostate cancer. Some medical researchers interpreted the small increased risk noted in the 1993 studies as a weak association that may be due to chance or bias. A systematic review of the medical literature in 1998 (Fertility & Sterility, 70: 191) further documented the lack of a significant relationship between vasectomy and prostate cancer. Additional convincing evidence of no relationship has been published in the Journal of Urology in June 1999 (161: 1848-1853), in the Journal of the American Medical Association in June 2002 (287:3110-3115), in the Journal of Urology in October 2002 (168: 1408-1411), and in Fertility and Sterility in November 2005 (84:1438-1443). A more recent study in 2014 raised the question once again, and once again, careful analysis of all available research data showed no association of vasectomy with prostate cancer. Studies as recent as 2016, show no increased risk of prostate cancer after vasectomy. The official position of the American Urological Association is that the association between vasectomy and prostate cancer risk is so weak that it need not even be discussed as part of routine pro-op counseling (see AUA Guidelines, pages 14-15). There are greater increases in the risk of prostate cancer (and mortality) associated with consuming milk/dairy products (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8255404/), meat (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8859108/#:~:text=Consumption%20of%20processed%20meat%20might,not%20with%20advanced%20prostate%20cancer) and alcohol (https://pubmed.ncbi.nlm.nih.gov/27842506/) or even having multiple sexual partners and not ejaculating often enough (https://pubmed.ncbi.nlm.nih.gov/30122473/).
The question of an association between vasectomy and subsequent cardiovascular disease was raised back in 1978 and 1980 by two studies which reported an increase in atherosclerosis (hardening of the arteries) in vasectomized laboratory monkeys. The last article listed above (Cancer and cardiovascular disease after vasectomy: an epidemiological database study. Fertility and Sterility 84:1438-1443, November 2005) provides an excellent bibliography of studies showing no association in humans as well as its authors' own data comparing 24,773 vasectomized men with 159,480 non-vasectomized men as a control group. Their findings "strengthen the evidence that vasectomy is not followed by an increased risk of myocardial infarction [heart attack], coronary heart disease as a whole, or stroke. In particular, we add strong support to the evidence that there is no elevation of risk of cardiovascular disease in men after long periods after vasectomy."
My office has copies of these and other research studies, available to any patient upon request.
If you are less than 30 years old and you have had fewer than 2 children, please consider the following points before having a vasectomy:
- You may regret it. Men who have vasectomies when they are in their 20's, especially if they have had fewer than two children, may be the ones most likely to seek vasectomy reversal at a later date, often regretting their vasectomy decisions if their reversals are not successful.
- You may change. Many men who think they will never want children when they are in their early 20's are delighted with fatherhood when they are in their 30's. You may be totally convinced now that you will never want children, but people change and you may have a much different outlook 10 years from now.
- Women change. Similarly, women who have no desire for children when they are in their early 20's may have a much stronger desire when they are in their 30's and when many of their friends are having children of their own.
- Relationships end. Since more than 50% of American marriages end in divorce, you may not be with the same partner ten years from now and a new partner may have a much stronger desire for children than your present partner does. So just because your present partner claims that she will never want children, her tune may change 10 years from now, or she may not even be your partner 10 years from now.
- The philosophy of you and your partner with respect to abortion should be considered. If you are both not philosophically opposed to abortion, you have some back-up should other forms of contraception fail, and having a vasectomy now may not seem as critical to avoid an unintended pregnancy. But keep in mind that if she gets pregnant, the choice is hers.
- Vasectomy should be considered a permanent and non-reversible procedure because vasectomy reversals are not always successful. So before having a vasectomy, know all of the other options ... HERE and HERE.
- Young men should consider Sperm Storage. The companies who provide the service will send what you need directly to your home, you can collect the semen specimens in the privacy of your home, and you can mail them back to the company in the storage container provided. Imagine meeting a prospective partner years after your vasectomy. You fall very much in love with her, but you know that she will someday want children. You can tell her, "I have had a vasectomy", or you can say, "I have had a vasectomy, BUT I banked sperm for future use." Now, which do you think will sound better to her? In her eyes, either you did a foolish thing years ago, or you made a responsible decision with good foresight. In one case, you may lose the girl; in the other case, you win her heart. So sperm storage can be a very smart thing, well worth the investment.
- Have you discussed your decision with your parents? If not, consider this: You're an adult, yes, but they helped you get there. How would you feel if your son came home one day and said that he had had a vasectomy? That he had done something to limit his future potential (to be a father) and to limit your own potential (to be a grandfather). How would you feel, after nurturing and guiding him for over two decades, if he did something to profoundly influence his future, but did not have the respect or courtesy to just tell you about it beforehand? As with many decisions in life, change the question from, "Should I tell my parents?" to "What can I do that I will never regret?" Would you ever regret not telling them? Possibly, especially if they are hurt as I, as a parent, would be. Would you ever regret telling them? Probably not. Having a vasectomy is still your decision, but at least you granted them the respect of letting them render an opinion. And if they succeed in discouraging you, because they know you better than any doctor does, you may one day thank them. If they don't succeed in discouraging you, they may split with you the cost of sperm storage and feel much better about your vasectomy in doing so.